Quick Summary
- Dementia is a general term for various diseases with different causes. Risk factors are mainly old age, genetic predisposition and an unhealthy lifestyle.
- Dementia is affecting more and more people in Switzerland, impacting both, patients as well as their relatives. This trend is expected to get worse in the future.
- It is crucial to identify the disease early on and take precautions. Switching to a healthier lifestyle can considerably slow down its progression.
- Advance care directives and patient decrees are legal tools to take precautions in the event of a dementia diagnosis.
What is dementia and what causes it?
‘Dementia’ is a general term for the continued or advanced decline of memory, thought or other cognitive abilities. In medicine, there are over 50 known manifestations of the disease. Alzheimer’s caused by a build-up of proteins, or vascular dementia triggered by reduced blood flow to the brain are particularly widespread. Certain forms of dementia cause nerve cells in the brain to die, which results in the decline in mental capacity.
The causes of dementia can vary. The main factor for developing dementia is old age. As a result, most dementia cases occur in people over 70 (so-called senile dementia). Other factors, such as genetic predisposition, pre-existing conditions, medication, alcohol and tobacco consumption or a lack of exercise in daily life can also affect the progression of the disease.
A distinction is made between primary and secondary dementia. Primary dementia is an independent disease (such as Alzheimer’s), which causes the decline in mental capacity. Secondary dementia, on the other hand, is the result of other illnesses, such as metabolic disorders or addiction.
How widespread is dementia in Switzerland?
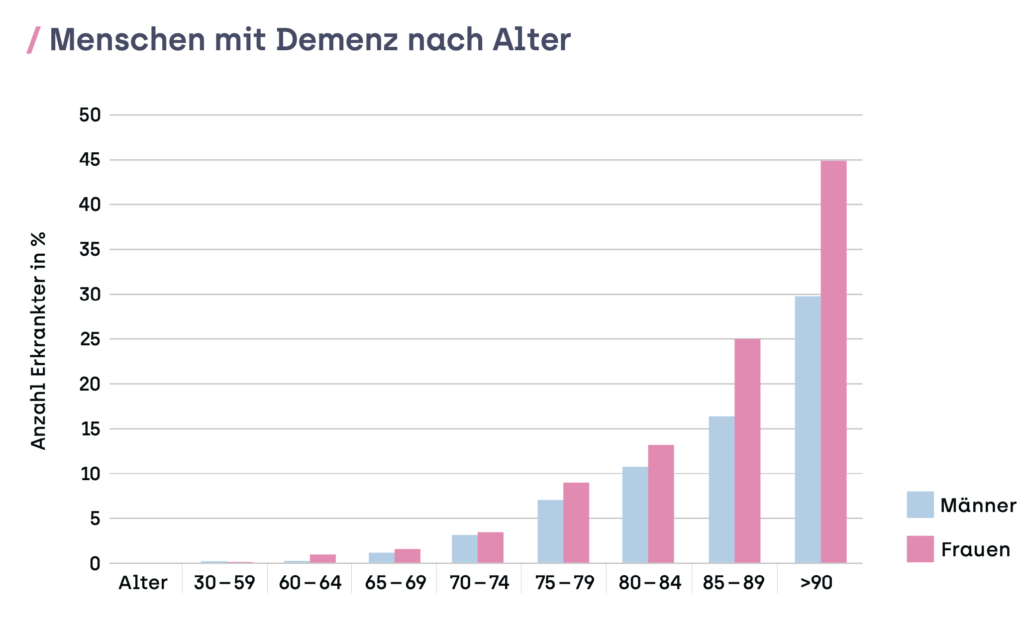
As the average age of the Swiss population increases, more and more people are being diagnosed with dementia. According to statistics from Alzheimer Schweiz, 144,300 people in the country suffered from dementia in 2020. Almost two thirds of them are women and only half of them were diagnosed by a specialist. According to estimates, the number of people with dementia will double to around 300,000 by 2040.
Dementia not only affects those suffering from the disease but also their close relatives, who are often faced with caring for them. Since dementia is increasingly becoming a widespread disease, the Swiss health care system is presented with enormous challenges. However, this also means that the Swiss population is developing a better understanding of what dementia patients need. In order to make long-term improvements to the support, care, welfare and treatment of people with dementia, the Federal Office for Public Health (BAG) developed a National Dementia Strategy from 2014 to 2019. A National Dementia Platform is currently being developed by the federation and the cantons based on the results.
How to recognise dementia
The symptoms of dementia are as diverse and dynamic as the causes. They also vary from person to person, which means it is not always easy to make a diagnosis. Typical initial symptoms include a slight, barely noticeable decline in cognitive abilities that become worse over time. Patients with Alzheimer’s exhibit a gradual loss of short-term memory and the ability to concentrate. With vascular dementia, people often have a stepwise progression of their symptoms. Later on, these symptoms progress to affect long-term memory, so dementia patients find it more and more difficult to differentiate between the past and the present. They forget memories of past experiences, and some dementia patients sometimes do not recognise their own relatives any more.
Why is it important to recognise dementia early on?
Considering these prospects, it is difficult for patients to accept the diagnosis of dementia. However, there are many good reasons to act early on. One good reason is to ease the burden on the relatives and taking precautions in the event of a lack of capacity of judgement, as dementia can affect the capacity of judgement and therefore testamentary capacity in those suffering from the disease. An advance care directive and a patient decree are legal tools to sort out personal care, wealth management, representation in legal cases as well as agreeing to medical treatments in the event of a permanent lack of capacity of judgement.
It is just as important to recognise dementia early on so that preventative measures can be taken: Being aware of the risk of dementia is the only way to specifically address factors that contribute to the progression of the disease – ideally under medical supervision. These factors include high blood pressure, obesity and high cholesterol levels. The most effective ways to prevent dementia are both simple and well-known: an active lifestyle, exercising outdoors as well as eating a healthy diet with plenty of fruit, vegetables, fish and whole grains. Brain exercise – crosswords, Sudoku or card and board games – also help to keep the body and mind fit and healthy. Maintaining social contacts is also extremely important: regular contact and talking with friends and relatives not only improves quality of life, but is also proven to boost mental health.
You might also be interested in
- II: The progression of dementia
- III: How testamentary capacity is assessed in people with dementia
- IV: Consequences of a lack of testamentary capacity in people with dementia
- V: Checking a will if the testator has dementia
- Your husband has dementia: ‘It was like a punch to the gut’
- Dementia: ‘All needs must be met immediately’
- Dementia: When a husband becomes a child
- Lack of capacity of judgement – what precautions should I take?
- Advance care directive and patient decree – do I need both?
