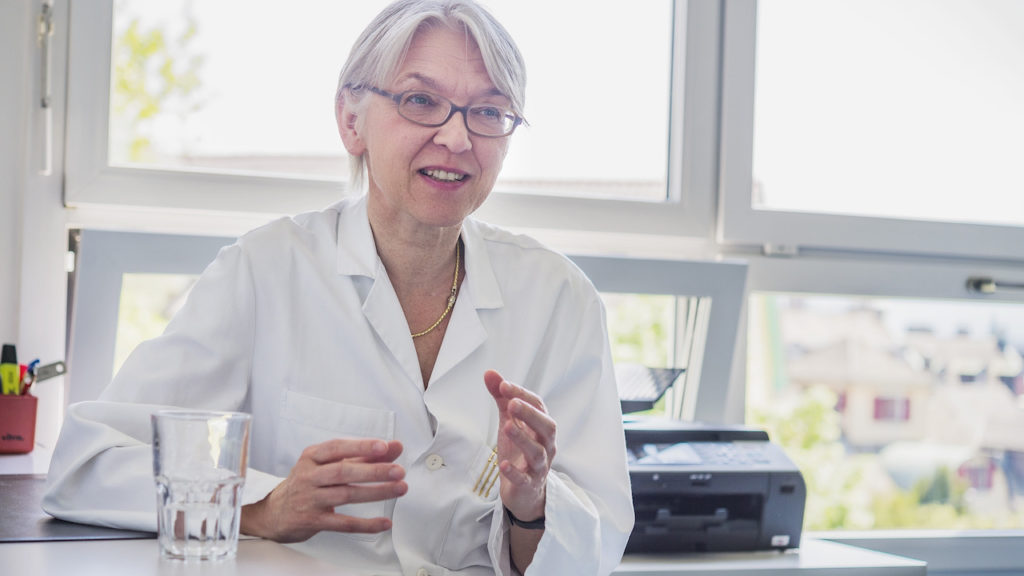
Ms Bergsträsser: You work as a senior physician at the Children’s Hospital Zurich and lead the Competence Centre for Palliative Care. Please tell me about your work.
PD Dr. Eva Bergsträsser: The following is important to me: We do not only care for terminally ill children and young people in their last days, hours. Our work begins much earlier. Sometimes right after birth. And it can last several years.
A significant difference to Adult Care.
Exactly. Palliative care for adults is much more end-of-life focused. We care for children of all age groups, from newborns to eighteen year olds, sometimes even older. Sometimes – and I hope there will be more in the future – we look after children before they are born and, of course, after their parents as well.
Because you know that the child will need care once it is born?
Yes. Because the child has a disease which was diagnosed through genetic testing or imaging, and the parents are asked what they wanted? Should we do everything we possibly can or, if the illness is so severe, should we focus on giving comfort to the child and giving it a chance at life, but not forcing it to stay alive.

Individualising child care
The care of parents, relatives and siblings plays a central role in this.
In principle, this is how it is in palliative care for children. We focus strongly on families and on close relatives. We care for a significant number of children who are neurologically seriously ill and are unable to communicate verbally. So they cannot use spoken language to communicate to us what they need. Therefore, communication often happens via the parents, sometimes via the siblings.
And this care does not only take place in the Children’s Hospital?
No, no. It usually takes place where the child is most comfortable. This can be in the hospital – and it very often is. This can also be at home or in institutions for long-term care as well as in other clinics.
Who are you then contacted by?
Usually it is professionals or specialists and sometimes general practitioners or paediatricians, who contact us. Sometimes the Spitex for children refers patients to us, or parents contact us directly.
And that way you and the people from your team become the main persons of contact?
Not the main contact persons. Because these children suffer from diseases that definitely still need treatment and where there are usually still treatment options. If we have a child with a serious heart condition, for example, the cardiologists and heart surgeons take the lead – we only provide advice and support.

Being there when the child and family need you
And you and your team accompany the family?
Yes. We provide comfort when needed. Sometimes people needs some, sometimes they don’t. We coordinate and accompany.
You and your team put a lot of heart and soul into this work. This creates trust and people feel more comfortable calling us at «inappropriate» times and asking for support.
This is our aim. We want to be informed early so that we can build a relationship of trust with the child, its parents and siblings.
And the families, do they then actually call at «inappropriate» times?
They can and they should. At night and on weekends. Patients know that the Kispi-phone is often with us at home.
Does the relationship end when a child dies?
Usually it does. After the death of the patient, my medical mandate ends. That is formally the case. We have professionals trained in psychology in our team and offer aftercare and support for grieving people There are many different offers.
Relationships are built. These can be more or less intense …
Yes. And I cannot just stop the communication. In certain cases, I was very close to the people and to the families. Then it is a matter of finding a humane as well as a professional ending. An ending that suits the needs of the families and also matches my resources, which are not unlimited.

Donations enable our work.
You need to be able to distance yourself emotionally.
Exactly. Usually, this works well. People know how busy I am.
How is your work financed?
Well, it’s not just about the funding our work, but also the one of the staff, for example. Half of it is covered by donations.
Your work can never be cost-effective.
Correct. We rely on the fact that a part of the work of the secretary, the doctors, psychologists, social workers and so on is financed by donations.
In addition, many of the services you provide to parents and relatives are not charged.
Yes. There are offers for siblings, relatives and the families that we cannot charge for. No health insurance and no insurance company covers these services.
Dr Bergsträsser, you talk to people about life and death. How does this affect your life?
It’s not only hard, it’s also beautiful. If people manage to successfully move from struggling to find therapy and a cure to accepting a serious illness and a shortened life, it can be a more peaceful and somewhat happier experience.
Despite the tragic fate?
Yes, if we succeed to improve the quality of life with palliative care. It is good to see a family not running from doctor to doctor, but using the remaining time to do something for the sick child and their family. Something that helps to deal with the loss later. But of course, there are also difficult moments. For example, if the care lasted for weeks, if it took place day and night, around the clock. That exhausts one both physically and emotionally.
Sometimes a hug has to be allowed.
It is necessary to keep distance.
Yes. And that is so for me and for my personal life, for example for my husband. I don’t want to burden him with my sad experiences from work all the time, and yet they are nevertheless noticeable. I may feel sad because something doesn’t work out.
One has to accept that life is unfair.
You experiences injustice all the time.
If someone doesn’t speak the language or has a migrant background, does that make your work more difficult?
It depends. There are young patients who cannot communicate verbally and there are parents who do not understand the language we speak. There are many ways of communication, and it can be incredibly powerful. Some people are not able to accept death and realise that I respect this. Yet, I still accompany them on their way which then can result in a positive experience for them.
If you want to comfort someone in Corona times, you have to keep your distance. How has the epidemic affected your work?
Of course, I also feel the distance. And there are situations where keeping distance is not possible. With me, no one has to cry behind a mask. I keep my mask on. And when it’s a difficult situation, I also give parents a hug. This has to be. With this I do not oppose the Corona protective measures, but I stay human.
To conclude: What do you wish for society to change when it comes to living and dying?
There is still a certain taboo surrounding the incurability of diseases. I would like to see more openness in this regard. Such difficult, tragic events should be given more importance. Parents, families and especially siblings who have had to experience such a loss deserve support and compassion.
Dr Bergsträsser, thank you for talking to us on the phone and for the photos provided by the Children’s Hospital Zurich.
Interview: Martin Schuppli, Photos: Children’s Hospital Zurich
The Children’s Hospital Zurich is a partner of DeinAdieu. Link to the profile: